INTRODUCTION
This guideline presents recommendations for assessment of pain in adult patients with life-threatening conditions such as cancer.
IASP defines Pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage”. Total pain encompasses physical, psychological, social, and spiritual aspects. More than 2/3rd of advanced cancer patients experience pain. Hence relief of pain should be an integral part of “Total care” concept of palliative care. The aim of a comprehensive pain assessment is to get an accurate description of pain and thus be able to identify the aetiology/pathophysiology of pain.
Note: pain is often poorly assessed and inadequately managed in people with dementia, learning disabilities or a stroke – seek specialist advice.
RECOMMENDATIONS
- Routinely screen all patients for the presence of any type of pain during every consultation/visit.
- Patient’s self-report should be the primary source of assessment.
- Comprehensive pain assessment on those with pain should be undertaken using validated pain assessment tools based on their applicability within the patient population.
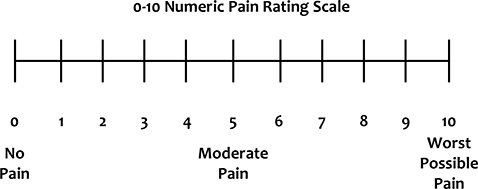
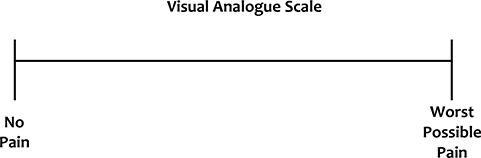
- The recommended pain assessment tools are visual analogue scale, verbal rating scale and numerical pain rating scale.
- If the patient is unconscious or cognitively impaired, observe for discomfort or other pain related behaviour (facial expressions, body movements, vocalisation, changes in routine).
- With the available information identify the type of pain – nociceptive or neuropathic. Signs and symptoms of neuropathic pain include; burning nature of pain, radiation, allodynia, hypoaesthesia, hyperalgesia, altered thermal threshold
- Identify the aetiology of pain and consider relevant investigations (if necessary) Explore the person’s beliefs, knowledge and level of understanding about pain and pain management.
- Document pain assessment on standardized forms.
- Reassessment of pain should be done on a regular basis – at least daily (if uncontrolled pain); in a home care setting this should be undertaken at least once in 48-72 hours.
- Record the patient’s pain and the responses to the pain management plan on an ongoing basis.
- Different pains and every new pain should be assessed separately.
ASSESSMENT
Assessment must determine the underlying cause of pain, severity, effectiveness of treatment and impact on quality of life for the patient and their family.
History (refer to the Guideline – Symptom Assessment)
Physical examination
- General examination
- Musculo-skeletal examination
- Neurological examination
- Local focused examination as appropriate
Investigations
- Cotton wool and artist’s brush for dynamic mechanical allodynia
- Blunt needle for hyperalgesia
- Appropriate radiological investigations (e.g. Plain radiographs of bone/bone scintigraphy – in case of pain due to suspected bone metastases/pathological fracture, MRI spine in case of suspected spinal cord compression)
Assessment Scales

REFERENCES
- Edmonton Symptom Assessment System [PDF file]. Retrieved from https://www.cancercareontario.ca/sites/ccocancercare/files/assets/CCOESAS-English.pdf on 28 April 2020
- Fallon, M., Hanks, G., Cherny, N. (2006). The principles of control of cancer pain. ABC of Palliative Care (pp. 4-7).
- Fink, R. Pain assessment: the cornerstone to optimal pain management. BUMC Proceedings. (2000); 13:236-239
- Haefeli, M. and Elfering, A. Pain assessment. Eur Spine J. (2006); 15: S17-S24. DOI 10.1007/s00586-005-1044-x
- Rayment, C. and Bennett, M.I. (2015). Definition and assessment of chronic pain in advanced disease. Oxford Textbook of Palliative Medicine (pp. 519-524)
- Visual Analogue Scale [PDF file]. Retrieved from http://img.medscape.com/article/742/580/VAS.pdf on 4 December 2018

If you have a query or comment you would like to share, please email us at guidelines.palcareindia@gmail.com


